COVID-19 Post-Acute Recovery:
Implications of health disparities on recovery for severely impacted patients
Publish Date: November 2020
Table of Contents:
Introduction
Patient Cohort
Outcomes
Discussion
References
Download the Full PDF Version
Introduction
At the height of the COVID-19 global pandemic in Connecticut, Hospital for Special Care (HFSC) converted its close observation unit, comparable to an intensive care unit, to a 10-bed COVID-19 recovery unit. This created a critical resource within the statewide health care system, a system that was overwhelmed with hospital admissions[i] and facing a post-acute environment that largely had no capacity to care for new COVID patients safely.
A multidisciplinary clinical team assigned to the HFSC COVID-19 recovery unit has conducted a detailed analysis of the patient cohort admitted, including racial and ethnic composition, age, gender and pre-COVID health status, as well as functional, cognitive and psychological measures of recovery. This analysis:
- underscores observed disparities in COVID-19 severe infection rates in communities of color
- addresses the implications of health disparities on recovery for severely impacted patients in the near and far-term
The analysis also demonstrates the impact of the long-term acute care hospital in ensuring equity in access to highly specialized, multidisciplinary care for severely impacted patients. This, and other data, will also inform a larger study conducted by the National Association of Long Term Hospitals (NALTH) documenting care outcomes at this level of care nationally.
Patient Cohort
Forty-one patients were admitted to HFSC’s 10-bed COVID-19 recovery unit between April and September 2020. Each patient met the referral criteria to qualify for intensive rehabilitation at the long-term acute level of care HFSC provides: all patients were admitted directly from an intensive care unit severely deconditioned, 83 percent had spent more than 96 hours on a ventilator and most had been hospitalized for at least a month prior to admission. In addition to caring for patients recovering from COVID-19, HFSC has operated at surge capacity (above its licensed bed-capacity) with approval from the Connecticut Department of Public Health throughout much of the pandemic expanding service to other pediatric and adult patients with complex medical conditions.
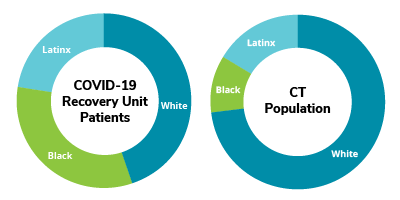
Patients ranged in age from 30 to 90 or older with a median age of 60. Seventy percent of patients in the cohort were under the age of 65. The median age of patients of Latinx ethnicity was lower than other subgroups in the cohort, a difference also reflected in the Connecticut population. Males were overrepresented in the cohort population (56 percent) as compared to the state population (48.8 percent).
Outcomes
Observed disparities:
The data observed within the HFSC COVID-19 patient cohort from April through September 2020 provides further evidence that historic disparities in access to health care and risk prevalence tied to race, ethnicity and socio-economic status have shaped patient experience of COVID-19. Patients of Black and Latinx racial and ethnic background and patients eligible for Medicaid were disproportionately represented among the most severely impacted by COVID-19 infection – and left post-acute care with recovery outcomes consistent with other patients in the cohort. They also left, however, with many of the same metabolic risk factors that increased their susceptibility to the coronavirus.
HFSC successfully eliminated the impact of each of race, ethnicity and insurance coverage variables on functional recovery from COVID-19 severe infection, demonstrating outcomes undifferentiated by demographic or socioeconomic barriers. In the near-term, is the capacity to mitigate the impact of health disparities on recovery is a critically important outcome and one that raises questions that merit longer-term study in the local and national health conversation.
Race/Ethnicity
- Individuals of Black or Latinx racial or ethnic background were disproportionately represented in the patient cohort requiring intensive post-acute care at HFSC following COVID-19 infection and disproportionately represented among Medicaid recipients in the patient cohort.
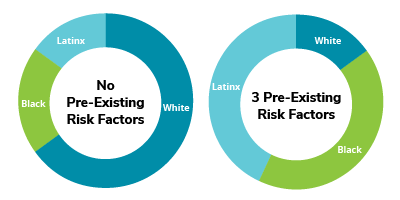
Pre-Existing Risk Factors
- A disproportionate number of patients of Black or Latinx racial or ethnic background had multiple, pre-existing risk factors for severe illness (including diabetes, obesity and hypertension) as compared to White patients in the cohort.
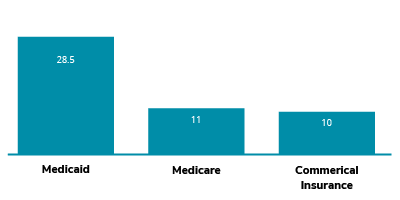
Relation of Insurance and Days on Vent in Acute Care
- Patients covered by Medicaid spent more days on a ventilator in acute care prior to admission at HFSC (median 28.5 days) than did patients with Medicare (median 11 days) or commercial insurance (median 10 days). The number of days a patient required mechanical ventilation is an indicator of how severely COVID-19 impacted their lungs.
Recovery Outcomes:
- Patients in the COVID-19 recovery cohort demonstrated substantial progress achieving a modified level of independent functioning for multiple daily activities.
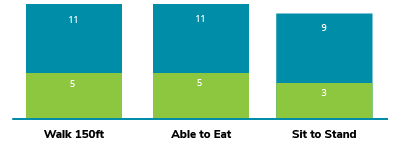
- Despite observed disparities within the composition of the patient cohort on admission, no subgroup differences in functional gains based on race/ethnicity, insurance coverage or metabolic risk factors were recorded at discharge as measured by FIM[ii]
- Among patients returning for outpatient care post-discharge, individuals of Black or Latinx racial or ethnic background reported less improvement in anger, fatigue, depression and anxiety than their White peers as measured via PROMIS® (Patient Reported Outcomes Measurement Information Systems). A recent study published in the Lancet Psychiatry Journal documented greater post-illness diagnoses of anxiety disorder, insomina and even dementia among COVID-19 patients.[iii]
Discussion
Rehabilitation and Recovery:
A comprehensive, multidisciplinary care team provided coordinated treatment for all patients within the COVID-19 patient cohort. The team differs from the clinical teams in acute care and other post-acute environments such as nursing homes, in both composition, and depth of experience providing intensive rehabilitation to severely deconditioned, pulmonary-compromised patients, under isolation precautions.
The HFSC COVID-19 recovery unit team included:
- Infectious disease preventionists and specialists
- Neuropsychologists
- Nurses and certified nursing assistants
- Occupational therapists
- Pastoral care
- Physiatrists
- Physical therapists
- Pulmonologists
- Registered dieticians
- Rehabilitation psychologists
- Respiratory therapists
- Speech language pathologists
- Therapeutic recreation specialists
Members of the clinical team, and all ancillary staff supports, received extensive training or re-training in donning and doffing of personal protective equipment, were fitted for N-95 masks, and followed extensive safety protocols to reduce infection transmission. Where possible, staff were either dedicated to the unit, or treated patients on the unit via telehealth or at end of shift.
The average length of stay for patients in the COVID-19 cohort was 29 days. Patients demonstrated some cognitive difficulty during their rehabilitation period (more than 1.5 standard deviations from mean). Among patients able to complete a cognitive screening, test scores showed 14 percent with lower than average attention and 68 percent with lower than average memory functioning. These observations are consistent with studies that have identified cognitive problems during inpatient rehabilitation after severe illness requiring an ICU level of care). A recent study published in the Lancet Psychiatry Journal documented greater post-illness diagnoses of anxiety disorder, insomina and even dementia among COVID-19 patients.[iiii]
A relatively low percentage of patients, as compared to the patients receiving intensive post-acute care not related to COVID-19, reported atypical levels of persisting pain (two percent), sleep disturbance (27 percent), fatigue (12 percent) or emotional distress (anger – seven percent; anxiety – 22 percent; depression two percent). Of note, among patients returning for outpatient care post-discharge, individuals of Black or Latinx racial or ethnic background reported less improvement in anger, fatigue, depression and anxiety than their White peers as measured via PROMIS® (Patient Reported Outcomes Measurement Information Systems).
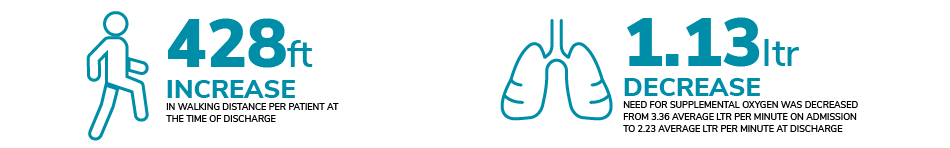
Patient progress in physical rehabilitation measured using the Functional Independence Measure, or FIM, was assessed based on ratings at time of admission and discharge. Patients, across all demographic and risk factors, demonstrated substantial progress from dependence on another person to a level of modified independence for basic acitivities of daily living. At discharge, patient need for supplemental oxygen was substantially decreased from 3.36 average liters per minute on admission to 2.23 average liters per minute. In addition, the average increase in walking distance per patient at the time of discharge was 428 feet.
Patients experiencing COVID-19 infection at a level of severity requiring ICU care are at-risk for a prolonged recovery period, even beyond post-acute intensive rehabilitation. The HFSC COVID-19 recovery team continues efforts to monitor patients’ status and engage them in outpatient pulmonary follow-up and ongoing multidisciplinary rehabilitation. The distribution of patients geographically – patients were admitted from six of Connecticut’s eight counties as well as at least one other New England state – raises challenges in ensuring access to COVID-informed follow-up care.
These challenges may be compounded by transportation barriers and limited access to telehealth services for the disproportionate number of individuals of color enrolled in Medicaid among the patient cohort. Non-emergency medical transportation, funded by Medicaid, is available, however historic mistrust of the system, compounded by the increased logistical complexity created by the pandemic remain barriers. It is no longer simply inconvenient to sit in a waiting room for an extended period of time waiting for transportation – it has become a safety issue for patients and providers alike. Telehealth services are available for many types of care, but not all treatments can be delivered remotely and not all patients have equitable access to appropriate devices or internet services.
With appreciation to the Hospital for Special Care COVID-19 Outcomes Team for individual and collective efforts to support data-informed clinical care through multidisciplinary collaboration. Rebuilding lives…together.
By: Kavita Arya, Anita Baltayan, MS, CCC-SLP, Timothy Belliveau, PhD, ABPP, Alaina Breitberg Hammond, PsyD, Joanne Dinda, Kristina Dzwonchyk, CPFT RRT, AARC/AACVPR, Jennifer Farley, MBA, RT (R) (M), Pamela Held, RRT, ME.d, Erin Ives, Da McGraw, Robert Rosso, Jennifer Weed
Lynn Ricci, FACHE, President & CEO
William Pesce, DO, Chief Medical Officer
©November2020 Hospital for Special Care
Read the Full Study
References
[i] https://data.ct.gov/Health-and-Human-Services/COVID-19-Tests-Cases-Hospitalizations-and-Deaths-S/rf3k-f8fg Connecticut reported nearly 2,000 patient hospitalizations due to Covid-19 for much of April 2020.
[ii] Functional Independence Measure (FIM) is an 18-item, clinician reported scale that assesses function in six areas including self-care, continence, mobility, transfers, communication and cognition.
[iii] https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(20)30462-4/fulltext
[iiii] https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(20)30462-4/fulltext
